In peripheral and cranial nerve neuromonitoring cases, we are often asked to monitor those specific nerves and corresponding end organs. Many surgeons are using us for information in regards to EMG activity signifying nerve root injury or irritation. Others are using us for the identification of the nerve during exposure.
While there’s merit to using us for that purpose, I believe some may be doing so without considering the following:
- Free-run EMG activity is due to during and/or after the fact manipulation/trauma, which may be too late to prevent injury when using sharp surgical instruments.
- Identification of the nerve does not tell you about the ability of the nerve to conduct through the entire length in question.
Both are known shortcomings.
To really know the functional integrity of the cranial or peripheral nerve, you need to stimulate along the nerve proximal and distal to the operative site.
Peripheral and Cranial Nerve Neuromonitoring
Here’s an example:
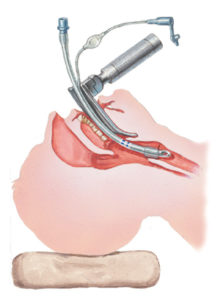
You’re monitoring free-run EMGs of bilateral recurrent laryngeal nerve in a thyroid cancer case and the surgeon has successfully stimulated and identified the nerve. However, the cancer is intrusive to the nerve, and identifying cancer vs nerve is difficult.
During surgery, the surgeon looks up at you panicked, and asked how things look. You tell him that EMG has been “quiet.” He stimulates the nerve and you let him know that you have a good response.
He sighs in relief and decides to continue to the other side based on the following facts:
- He knows that he has removed enough of the tumor on the first side
- The nerve did not show a typical response to irritation/injury
- He thinks he has an intact nerve since a compound muscle action potential (CMAP) was recorded
- He visualizes what he thinks is a nerve
But on the other side, his luck runs out. The nerve is encompassed in the tumor, and every time he tries to peel it off, train EMG sounds off. But since the first side is intact (or so he’s assuming with the peripheral nerve stimulation forming a proper compound muscle action potential), he feels a more aggressive approach is warranted to take as much tumor as possible. During the tumor removal, train EMG runs throughout, and then he’s finally done.
You’ve told him about the EMG, but it’s his decision to continue taking out this tumor.
And then… Yes! The train EMG has disappeared. The surgeon stimulates the second nerve again and it gives a proper CMAP.
Success!
The case got a little hairy there for a second. And as you wait for the patient to wake up, you agree with the surgeon that there would be no real surprise if the patient wakes up with vocal paresis because you utilized cranial nerve neuromonitoring. That one side did show signs of irritation, so having a temporary weakness isn’t out of the question.
But you both are surprised when the patient has complete vocal paralysis and the follow-up studies show that it was the first side with the complete nerve injury, not the side with the train EMG.
Oops.
And since he only stimulated distal to the lesion on the second side, he doesn’t know the extent of the integrity of that side’s recurrent laryngeal nerve. Or if there will be enough regeneration of the nerve to restore motor function to the vocal muscles.
Fingers crossed.
In my next post, I’ll go over how I would grade the person doing this hypothetical case (just like I do for myself in my own cases).
Here’s a hint… poor monitoring is probably worse than no monitoring at all.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...